It’s shocking, but about 15% of women face postpartum depression during their perinatal period. It’s a tough and complicated illness that so many new mothers go through, even though it’s not always talked about. We all know that motherhood is filled with overwhelming joy and nervousness, but to many women’s surprise, depression can sneak in too. If you’re feeling like something isn’t quite right, just know you’re not alone. In fact, you’re part of a larger community of women navigating the same emotional challenges, and we’re here to help you understand what the postpartum depression time frame really means, how to recognize it, and how to heal.
What Is Postpartum Depression?

Credit: marchofdimes.org
Let me tell you honestly, Postpartum depression (PPD) is more than just the “baby blues” that many new moms experience in the first few weeks after childbirth. It’s a serious mental health condition that affects a significant number of new mothers. It can make you feel isolated, hopeless, and even disconnected from your baby.
These feelings can last much longer than the fleeting “baby blues,” and they’re not a reflection of how much you love your baby. It’s just that your body and mind are trying to adjust to a big life change after childbirth.
I want you to remember: You are not alone, and this is not your fault. Postpartum depression is not a sign that you’re failing as a mother. It’s a health issue that can be treated with professional support, therapy, and sometimes medication. And trust me, reaching out for help is a strong and empowering choice. elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Key Points About Postpartum Depression
Onset: Symptoms typically show up within the first few weeks after giving birth, but can develop anytime within the first year.
Impact: PPD can deeply affect your ability to care for your baby, yourself, and manage day-to-day life.
Treatment: With the right treatment, including therapy and sometimes medication, you can begin to feel like yourself again.
It’s common: Around 1 in 7 women experience postpartum depression, so if you’re struggling, you’re not alone.
What Is Postpartum Psychosis?

Credit: picklesandicecreamga.org
Now, let’s talk about something a bit more intense: postpartum psychosis. While postpartum psychosis is extremely rare, it is serious and needs urgent attention. If you notice anything like hallucinations, delusions, or extreme mood swings, don’t wait to get help.
Postpartum psychosis usually comes on quickly, within the first two weeks after giving birth, and can be a medical emergency.
It’s so important that if you or someone you know is experiencing these kinds of symptoms, it’s crucial to get professional help immediately. Postpartum psychosis is very different from postpartum depression and can cause mothers to feel confused or unable to distinguish reality.
Onset: Symptoms generally start within the first two weeks after delivery.
Symptoms: Hallucinations, delusions, paranoia, confusion, and sudden extreme mood shifts.
Urgency: Postpartum psychosis is considered a psychiatric emergency and needs immediate medical attention.
Treatment: Often requires hospitalization and medical treatment, including medication and therapy.
Types of Postpartum Depression
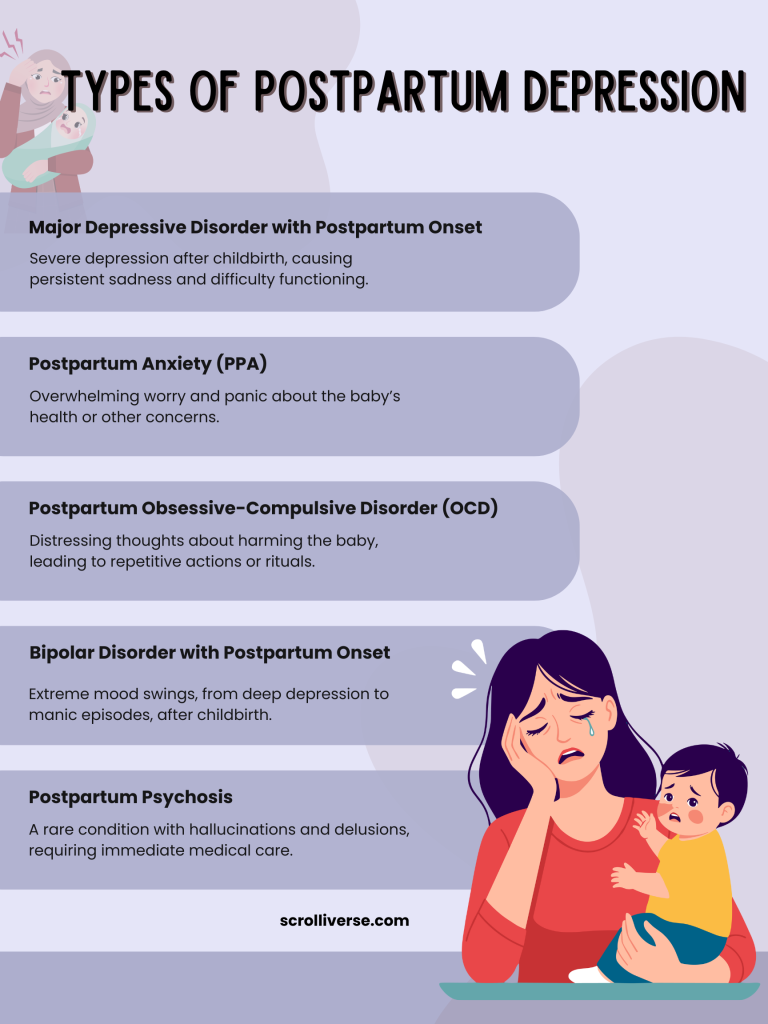
Now, the deal is that Postpartum depression doesn’t look the same for everyone, and it comes in different types. Understanding the various types of PPD can help you identify what you’re experiencing and seek out the best treatment. Here’s a deeper look into the different forms:
Major Depressive Disorder with Postpartum Onset
This is the most common form of postpartum depression. It’s marked by feelings of deep sadness, intense mood swings, and a complete lack of interest in activities that you usually enjoy. It may feel like you can’t connect with your baby or anyone around you.
This is not about being “tired” or “feeling off”; it’s a significant depressive episode that often requires professional treatment.
Symptoms Include:
Feeling hopeless or empty
Extreme sadness or tearfulness, without a clear reason
Difficulty bonding with your baby
Lack of energy or interest in things you once enjoyed
Thoughts of harming yourself (if you’re experiencing this, reach out for help immediately)
Anxiety with Postpartum Depression
Next comes anxiety, with postpartum depression can make you feel constantly on edge, worried, and unable to relax. This type of PPD is characterized by severe worry about your baby’s safety, your ability to care for them, or your own mental stability. You might feel like something terrible is going to happen, even when there’s no real cause for concern. The pressure of being a new mom can often heighten feelings of anxiety.
Symptoms Include
Excessive worry about your baby’s health or safety
Trouble relaxing, even when your baby is sleeping
Racing thoughts that don’t stop
Physical symptoms like tension, nausea, or heart palpitations
Feeling like you can’t breathe or focus
Postpartum Obsessive-Compulsive Disorder (OCD)
Do you know that postpartum OCD isn’t the same as the regular OCD? In this case, mothers often experience intrusive thoughts that they might harm their baby, even though they have no intention to do so.
These thoughts are often disturbing and cause immense guilt. To try to reduce anxiety, mothers with postpartum OCD may engage in repetitive behaviors or rituals.
Symptoms Include
Intrusive, distressing thoughts about harming your baby
Performing repeated actions or rituals (like checking the baby’s crib multiple times or washing hands excessively) to reduce anxiety
Feeling like you’re losing control
Strong fear of doing something dangerous without realizing it
Postpartum Post-Traumatic Stress Disorder (PTSD)
Some women experience PTSD after a traumatic birth experience. It might be due to an emergency C-section, complications during delivery, or simply feeling overwhelmed by the process. Postpartum PTSD is characterized by flashbacks, nightmares, and extreme anxiety around the birth event or your baby’s health.
Symptoms Include
Flashbacks or intrusive memories of the birth
Nightmares about the delivery or the baby’s health
Feeling emotionally numb or detached
Difficulty trusting others to care for your baby
Hyper-vigilance or feeling “on edge” at all times
Symptoms of Postpartum Depression

Credit: madisonwomenshealth.com
Well, postpartum depression symptoms can manifest in many ways, and their severity can vary in severity. For some women, it’s like a dark cloud that hovers, making everything feel heavy and difficult.
And for others, it might look like anxiety, guilt, or feeling detached from their baby or loved ones. It’s also possible to experience physical symptoms, like loss of appetite after childbirth, or feeling physically drained.
Persistent feelings of sadness or hopelessness
Extreme fatigue or lack of energy
Trouble bonding with your baby or feeling disconnected from them
Trouble concentrating or making decisions
Overwhelming feelings of guilt or inadequacy
Crying for no apparent reason
Changes in appetite or weight (like breastfeeding loss of appetite)
Sleeping too much or too little
Thoughts of harming yourself or your baby (please seek help immediately if you have these thoughts)
Postpartum Depression Time Frame and When to Expect Recovery

Credit: baptistonline.org
So, how long does postpartum depression last? Well, there isn’t a set time frame, as it varies from mother to mother. Some women may feel better within a few months, while others may struggle for a year or longer.
Knowing what to expect during the postpartum time after delivery can help you feel more in control of your journey toward healing.
When to Expect Symptoms
First Few Weeks: Many moms feel a little weepy or overwhelmed during the first couple of weeks after birth, often called “baby blues.” This is common and tends to pass within 10 to 14 days.
First 3–6 Months: If symptoms of sadness, fatigue, or anxiety persist beyond this time, you might be dealing with postpartum depression. Professional treatment can help during this phase.
Long-Term Recovery: With proper treatment, most women start feeling better between 6 to 12 months after giving birth. However, some may need longer, and that’s okay too.
Recovery Timeline
Immediate Action: The sooner you reach out for help, the faster you can start feeling better. The earlier treatment starts, the better the outcomes.
First 6 Weeks: Some women begin to notice improvements after the first few weeks of therapy or medication.
3-6 Months: Many moms start to feel like themselves again during this time. The right treatment can really make a difference.
1 Year: If PPD continues after a year, it’s a good idea to revisit your treatment plan with your doctor to find what works best.
Causes of Postpartum Depression
Honestly speaking, the causes are complex, and they can be influenced by a number of risk factors for postnatal depression.
There’s no single cause of PPD, but a combination of physical, emotional, and psychological factors plays a role.
It’s not something you can control, and it doesn’t mean you’re not strong enough to handle motherhood.
Hormonal Changes: After childbirth, your hormone levels plummet, which can affect your mood and emotions.
Sleep Deprivation: Not getting enough rest due to the baby’s feeding schedule or nighttime awakenings can contribute to feelings of depression.
Previous Mental Health Issues: If you’ve had depression, anxiety, or other mental health struggles before pregnancy, you might be at a higher risk.
Stressful Life Events: Challenges like relationship stress, financial strain, or a difficult pregnancy or delivery experience can make the transition to motherhood harder.
Lack of Support: Not having enough emotional or physical support can cause feelings of isolation and frustration.
Baby Blues vs Postpartum Depression
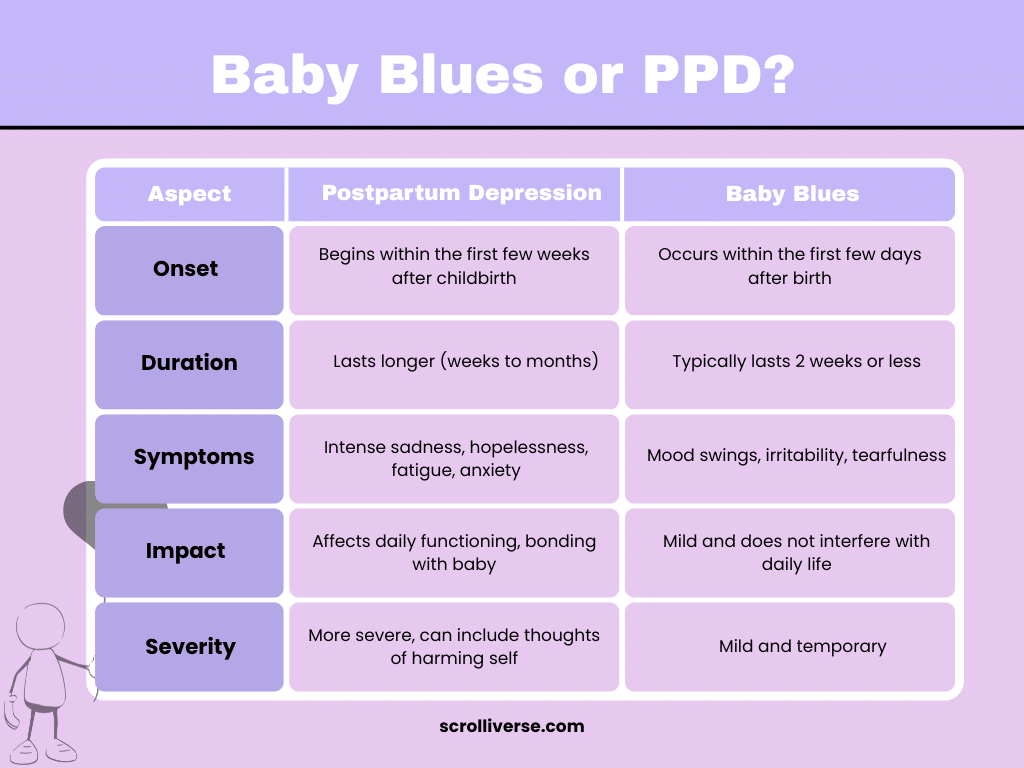
The baby blues are common and affect most new moms. It involves mild sadness, mood swings, irritability, and fatigue. But it’s short-lived and usually resolves within a couple of weeks. On the other hand, postpartum depression lasts longer, is more intense, and interferes with your ability to function.
Baby Blues: Temporary, mild mood swings, feeling weepy, and emotional (usually lasts for 2 weeks).
Postpartum Depression: Persistent feelings of sadness or hopelessness that interfere with your daily life, lasting for weeks or months.
Diagnosis and Treatment
Diagnosing postpartum depression typically involves a healthcare provider asking about your symptoms, emotional well-being, and mental health history. Postpartum depression treatment can include therapy, medication, and lifestyle changes. The key to feeling better is finding a treatment plan that works for you.
Therapy: Cognitive-behavioral therapy (CBT) and other forms of psychotherapy can help you manage your emotions and thought patterns.
Medication: Antidepressants may be prescribed if symptoms are severe or don’t improve with therapy.
Support Groups: Meeting with other mothers going through similar experiences can reduce feelings of isolation.
Lifestyle Changes: Prioritizing sleep, eating nutritious meals, and finding time for relaxation and exercise can help improve mood.
Support from Family: Having your partner or loved ones involved in your recovery can make a big difference.
Prevention and Risk Factors
While you can’t always prevent postpartum depression, there are things you can do to reduce your risk. Recognizing the early signs, getting support, and taking care of your emotional well-being are key to reducing the impact of PPD. For more tips and support, visit our guide for new moms.
Previous mental health struggles (e.g., depression or anxiety)
Lack of emotional support from family or friends
Stressful life events (like a difficult birth or financial problems)
Unplanned pregnancy or difficulties in bonding with the baby
Sleep deprivation
Preventive Measures
Prioritize your health: Take care of yourself by getting enough sleep, eating well, and moving your body.
Talk openly: Keep the lines of communication open with your partner, friends, or family. Let them know how you’re feeling.
Seek help early: The sooner you address your feelings, the sooner you can start healing.
Final Remarks
In a nutshell, postpartum depression is tough, but it’s not permanent, and it’s certainly not something you have to handle alone. There’s no shame in seeking help, and the sooner you do, the quicker you can start feeling like yourself again. Remember, you are doing an incredible job as a mother, and your mental health is just as important as your physical health.
Take it one day at a time, seek the support you deserve, and know that recovery is possible. You’ve got this, mama.
Frequently Asked Questions
Here’s what you need to know about the postpartum depression time frame.
How long does postpartum depression last?
Postpartum depression can last anywhere from a few weeks to over a year, depending on the severity and treatment.
Can postpartum depression go away on its own?
While some women may experience mild baby blues that go away on their own, postpartum depression typically requires treatment for full recovery.
What are the signs of postpartum psychosis?
It includes symptoms like hallucinations, delusions, and severe mood swings, and it requires immediate medical intervention.
Can postpartum depression affect bonding with my baby?
Yes, it can make bonding difficult, but with treatment and support, you can regain that connection with your baby.
Is it safe to take medication for postpartum depression while breastfeeding?
Many antidepressants are safe for breastfeeding mothers, but it’s important to discuss any concerns with your doctor before starting treatment.




















Leave a comment